Diverticulitis
Overview
Diverticulitis is inflammation of irregular bulging pouches in the wall of the large intestine.
Typically, the wall of the large intestine, also called the colon, is smooth. An irregular, bulging pouch in the colon wall is called a diverticulum. Multiple pouches are called diverticula.
Diverticula are common, especially after age 50. They are usually found in the lower part of the colon. Most often, they don't cause problems. The presence of diverticula is called diverticulosis. Diverticulosis isn't a disease condition.
When these pouches become inflamed, the condition is called diverticulitis. Inflammation is immune system activity that increases blood flow and fluids to a site in the body and delivers disease-fighting cells. Inflammation of diverticula can cause severe pain, fever, nausea and changes in your stool habits.
Mild diverticulitis is usually treated with rest, changes in your diet and possibly antibiotics. Severe diverticulitis usually needs antibiotic treatment in the hospital. Surgery may be needed for severe or frequent diverticulitis.
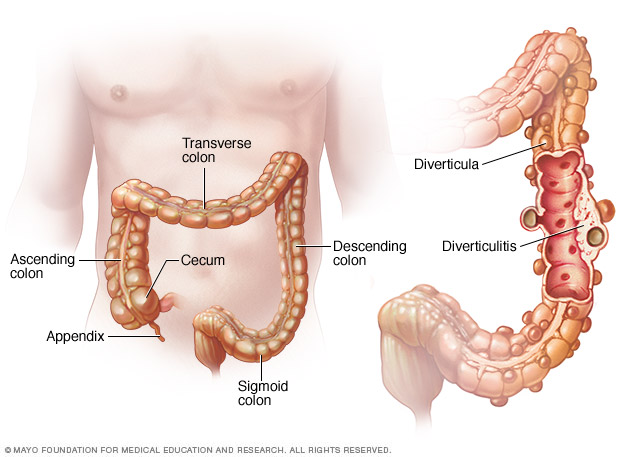
Diverticulosis occurs when small, bulging pouches (diverticula) develop in your digestive tract. When one or more of these pouches become inflamed or infected, the condition is called diverticulitis.
Symptoms
A common symptom of diverticulitis is pain in the area below the chest called the abdomen. Most often, pain is in the lower left abdomen.
Pain from diverticulitis is usually sudden and intense. Pain may be mild and gradually worsen, or the intensity of the pain may vary over time.
Other signs and symptoms of diverticulitis may include:
- Nausea.
- Fever.
- Tenderness in the abdomen when touched.
- Changes in stool, including sudden diarrhea or constipation.
When to see a doctor
Get medical care anytime you have constant, unexplained abdominal pain, particularly if you also have a fever and notable changes in stools.
Causes
Diverticula gradually develop over time in the walls of the colon. They are common in older adults. Pressure in the colon — possibly from spasms or straining — may cause diverticula to form where the wall of the colon is weak.
Diverticulitis is inflammation of one or more diverticula. This may happen because of bacterial disease or damage to diverticula tissues.
Risk factors
Diverticulitis is more common among people over 50. Other factors that increase the risk of diverticulitis include:
- Obesity.
- Smoking.
- A diet of low-fiber foods.
- A diet high in red meat.
- Heavy alcohol use.
- Lack of exercise.
- Low vitamin D levels.
- Certain medicines, such as steroids, opioids and nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
Complications
About 15 percent of people with diverticulitis develop complications. These may include:
- A pocket of pus from bacterial disease, called an abscess.
- Blockage of the colon.
- An irregular passageway, called a fistula, between the bowel and another organ in the body.
- A tear in the colon wall that allows waste to spill out, causing serious disease of the abdomen lining, called peritonitis.
- Bleeding from ruptured blood vessels, also called diverticular hemorrhage.
Prevention
To help prevent diverticulitis:
- Exercise regularly. Regular, vigorous exercise decreases the risk of diverticulitis.
- Eat a high-fiber diet. A high-fiber diet improves the movement of waste through the colon and decreases the risk of diverticulitis. Fiber-rich foods include fruits, vegetables, whole grains, seeds and beans. Cut back on red meats and sweets.
- Maintain a healthy weight. Talk to your healthcare professional or a dietitian about goals for a healthy weight for you and strategies to reach your goals.
- Drink plenty of fluids. Fiber works by absorbing water and increasing the soft, bulky waste in your colon. Drinking fluids improves the movement of waste and prevents constipation.
- Quit smoking and limit alcohol use. Smoking and heavy alcohol use are associated with an increased risk of diverticulitis.
In the past, healthcare professionals recommended that people with diverticulitis avoid nuts, seeds and popcorn. Studies have shown that these foods do not increase the risk of diverticulitis. Seeds and some nuts are good sources of fiber.
Diagnosis
A number of conditions can cause pain and other symptoms related to diverticulitis. Your health care professional will do an exam and order tests to determine the cause of symptoms.
During the physical exam, your healthcare professional will gently touch different parts of the abdomen to learn where you have pain or tenderness. An exam also may include a pelvic exam to test for disease of the female reproductive organs.
Laboratory tests may be used to rule out other conditions and make a diagnosis:
- Blood tests for signs of infection and immune-system activity.
- Urine test.
- Stool test.
- Pregnancy test.
- Liver enzyme test to rule out liver disease.
A computerized tomography (CT) scan can show inflamed diverticula, abscesses, fistulas or other complications.
Treatment
Treatment depends on how serious the condition is.
Uncomplicated diverticulitis
When symptoms are mild and there are no complications, the condition is called uncomplicated diverticulitis. If your symptoms are mild, you may be treated at home.
Your healthcare professional is likely to recommend a liquid diet. When symptoms begin to improve, you can gradually increase solid food, beginning with low-fiber foods. When you're fully recovered, you can resume a regular diet with high-fiber foods. A fiber supplement may also be recommended.
You also may have a prescription for antibiotics. You will need to take all of the pills even when you are feeling better.
Complicated diverticulitis
If you have serious symptoms or signs of complications, you'll likely need to be in the hospital. Antibiotics are given with an intravenous tube, also called an IV.
Surgery
Relatively simple procedures may be used to drain an abscess or stop bleeding related to diverticulitis.
Surgery on the colon may be needed if:
- You have had complicated diverticulitis.
- Complications include ruptures in the colon wall, fistulas or other serious tissue damage.
- You have had multiple episodes of uncomplicated diverticulitis.
- You have a weakened immune system.
Surgery is often performed through small openings in the abdomen. This procedure is called laparoscopic surgery. In some cases, surgery through a single, large opening is needed. There are generally two procedures for treating diverticulitis:
- The diseased section of the colon is removed. The remaining healthy tissues are connected to re-create a complete colon.
- The healthy section and diseased section are separated. The healthy section is directed to an opening in the abdomen wall. Waste is collected in a bag called a colostomy bag. This gives the diseased section time to heal. When it is healed, the two sections are reconnected, and the opening in the abdomen wall is closed.
Other surgical procedures may be necessary to treat complications such as peritonitis and fistulas.
Follow-up care
Your healthcare professional may recommend a colonoscopy six weeks or longer after you no longer have symptoms of diverticulitis. A colonoscopy is an exam used to look for irregular growths or cancer in the colon or rectum. A recommendation for this procedure depends on when you last had a colonoscopy and how serious your diverticulitis was.
Alternative medicine
A few small clinical trials found evidence that probiotic supplements to increase good bacteria in the colon may reduce risk of new episodes of diverticulitis. But there is not enough scientific evidence to show that probiotics should be used. Talk to your healthcare professional before taking a probiotic or other supplements.
Preparing for an appointment
You may be referred to a doctor who specializes in disorders of the digestive system, called a gastroenterologist.
What you can do
- Be aware of any pre-appointment restrictions, such as not eating solid food on the day before your appointment.
- Write down your symptoms, including any that may seem unrelated to your reason for the appointment.
- Make a list of all your medicines, vitamins and supplements, as well as the dose and reason for taking each one.
- Write down your key medical information, including other conditions.
- Write down key personal information, including any recent changes or stressors in your life.
- Ask a relative or friend to accompany you, to help you remember what the healthcare professional says.
- Write down questions to ask your healthcare professional.
Questions to ask your doctor
- What's the most likely cause of my symptoms?
- What kinds of tests do I need? Do these tests require any special preparation?
- What treatments are available?
- How can I prevent diverticulitis from coming back?
- Should I remove or add any foods in my diet?
- I have other health conditions. How can I best manage these conditions together?
In addition to the questions that you've prepared to ask your healthcare professional, don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your healthcare professional is likely to ask you a number of questions. You may be asked:
- When did you first begin experiencing symptoms, and how severe are they?
- Have your symptoms been continuous or occasional?
- What, if anything, seems to improve or worsen your symptoms?
- Have you had a fever?
- What medicines and pain relievers do you take?
- Have you had any pain with urination?
- Have you ever had a screening test for colon cancer called a colonoscopy?
Last Updated May 15, 2024
© 2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved. Terms of Use




